Cancer Risk After Total Hysterectomy: Understanding the Implications

Total hysterectomy is a significant surgical procedure that entails the removal of a woman's uterus and cervix. In some cases, it may also involve the removal of the ovaries and fallopian tubes. This procedure is often considered for a variety of medical reasons, including uterine fibroids, endometriosis, uterine prolapse, and certain cases of gynecological cancers. However, one of the pressing questions that women may have is regarding the cancer risk after total hysterectomy. This article aims to delve into this topic, providing a comprehensive understanding of the implications associated with this surgical treatment.
Understanding Total Hysterectomy
A total hysterectomy is often recommended when less invasive treatments have failed or when there is a significant risk of developing cancer. Removing the uterus and cervix can prevent various health issues, but it's vital to understand the surgical implications and potential health outcomes.
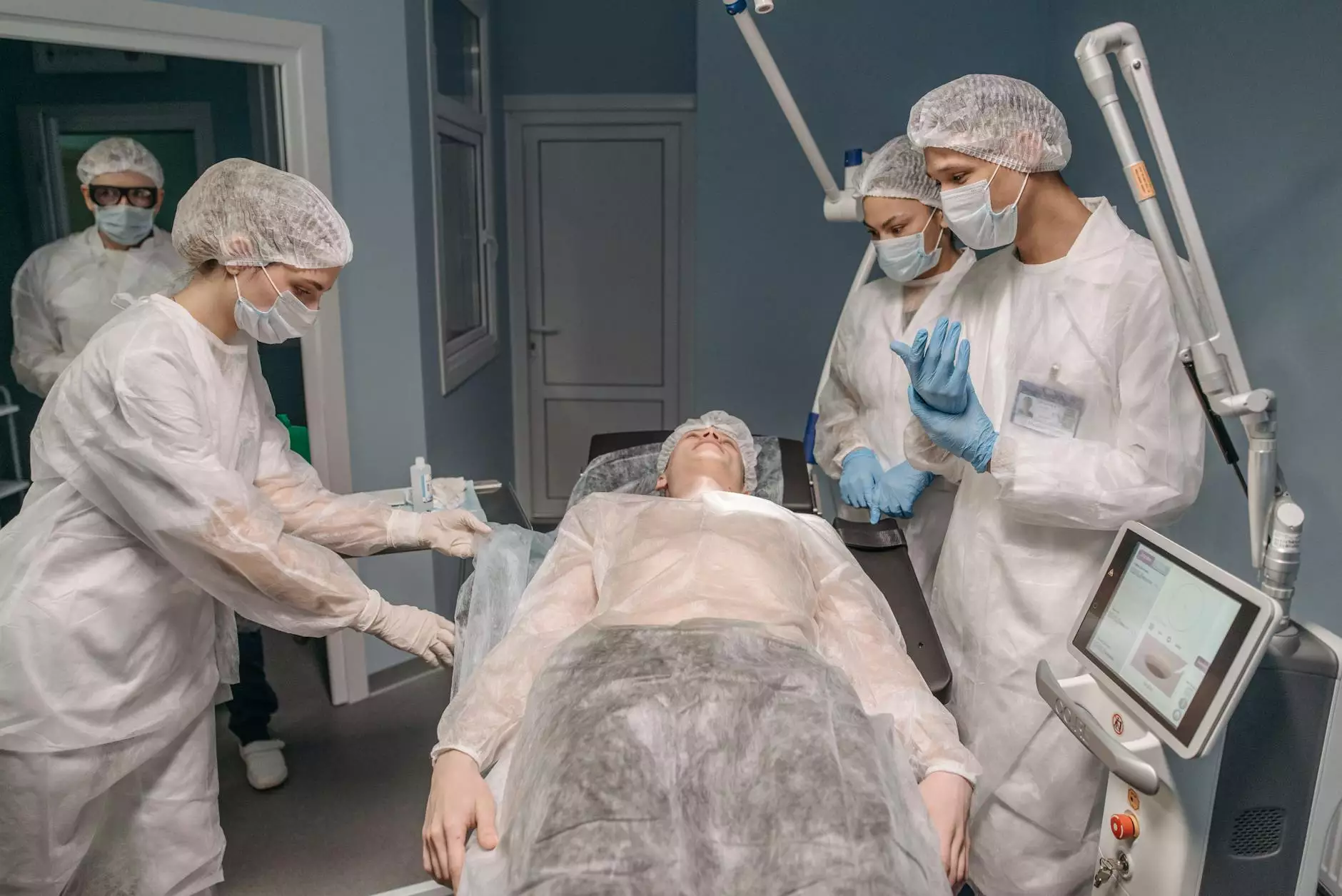
What Happens During the Procedure?
During a total hysterectomy, an obstetrician or gynecologist removes the uterus and cervix. The procedure can be performed through different surgical approaches:
- Abdominal Hysterectomy: Involves a larger incision in the abdomen.
- Vaginal Hysterectomy: Removes the uterus through the vagina, often resulting in less postoperative pain.
- Laparoscopic Hysterectomy: A minimally invasive approach using small incisions and a camera.
After surgery, the patient typically stays in the hospital for a few days, with a recommended recovery period of several weeks. The extent of surgery—whether the ovaries and fallopian tubes are removed—can impact recovery and hormonal balance.
The Link between Total Hysterectomy and Cancer Risk
One of the concerns for women undergoing total hysterectomy is the potential impact on cancer risk. It is crucial to understand how this procedure influences your overall health, including the risk of developing specific types of cancers.
Factors Influencing Cancer Risk
The relationship between total hysterectomy and cancer risk is complex and can be influenced by various factors:
- Age: Younger women may experience different risks compared to older women.
- Family History: A strong family history of cancer, particularly breast or ovarian cancer, can heighten individual risk factors.
- Genetic Factors: Genetic mutations, such as BRCA1 and BRCA2, play a significant role in cancer risk.
- Hormonal Changes: The removal of ovaries can lead to hormonal imbalances that may affect cancer risks.
Is There an Increased Risk of Cancer?
After a total hysterectomy, it is essential to consider the types of cancers that may or may not have increased risk. Research indicates:
Ovarian Cancer
If the ovaries are preserved, there may still be a risk of ovarian cancer, particularly if there is a family history or other contributing factors. However, if both ovaries are removed during the hysterectomy, the risk substantially decreases. Women should consult their doctors for personalized screening guidelines post-surgery.
Endometrial Cancer
Women who have a total hysterectomy eliminate the risk of developing endometrial cancer, as the uterus is removed. This is one of the primary reasons for opting for this procedure, especially in women at high risk.
Cervical Cancer
Removal of the cervix during a total hysterectomy also diminishes the risk of cervical cancer. Regular screenings such as Pap smears prior to surgery are essential in monitoring overall gynecological health.
Breast Cancer
While total hysterectomy does not have a direct impact on breast cancer risk, the hormonal changes post-surgery may influence some women depending on various factors including age and lifestyle.
Benefits of Total Hysterectomy
Despite concerns regarding cancer risk after total hysterectomy, this procedure offers several benefits that can significantly enhance a woman's quality of life:
- Relief from Symptoms: Women suffering from severe fibroids or endometriosis often experience relief from painful symptoms post-surgery.
- Prevention of Recurring Problems: For many women, the surgery can prevent the recurrence of conditions that negatively impact health and well-being.
- Peace of Mind: Removing reproductive organs can provide peace of mind for women at high risk for reproductive cancers.
Post-Operative Care and Monitoring
Following a total hysterectomy, patients must engage in appropriate post-operative care. This includes:
- Regular Check-Ups: Women should schedule regular follow-up appointments to monitor their overall health and address any concerns.
- Screening for Other Cancers: Depending on personal and family medical histories, regular screenings for breast and ovarian cancer may still be advisable.
- Managing Hormonal Changes: Women who undergo oophorectomy (ovary removal) will need to discuss options for hormone replacement therapy with their physicians.
Conclusion
In conclusion, while there are understandable concerns about cancer risk after total hysterectomy, the procedure is often necessary for the health and well-being of many women. With proper surgical consultation, understanding the implications of the surgery, and engaging in post-operative care, women can make informed decisions that align with their health needs and life goals.
Women contemplating a total hysterectomy should engage in thorough discussions with their healthcare providers, considering both the benefits and potential risks. By being proactive and educated, they can navigate their health journey confidently.
For more personalized advice and care, women may consult with professionals at Dr. Seckin's Clinic for their expertise in women's health and gynecological surgeries.